Medical Billing Explained
You work hard to provide the best care available to your patients. You exercise caution, best practices, and thoughtful consideration—leading to successful outcomes. Then you receive the HCAHPS survey or another patient satisfaction data form, and the numbers aren’t as high as you expect. Why? Because, after your patients are discharged, they receive medical bills that are difficult to understand, higher than expected, and unexplained.
American Healthcare Recipients Are Dissatisfied With Billing
A 2016 survey conducted by Copatient found that 72% of Americans are confused by their medical bills. In the same survey, 94% said they considered some medical bills they received to be too expensive. There is an opportunity here for hospitals, clinics and other medical facilities to increase patient satisfaction by explaining the billing process in greater detail. Patients deserve to know what they will be expected to pay before they receive treatment, and a little education can go a long way toward increased satisfaction.
The Medical Billing Cycle
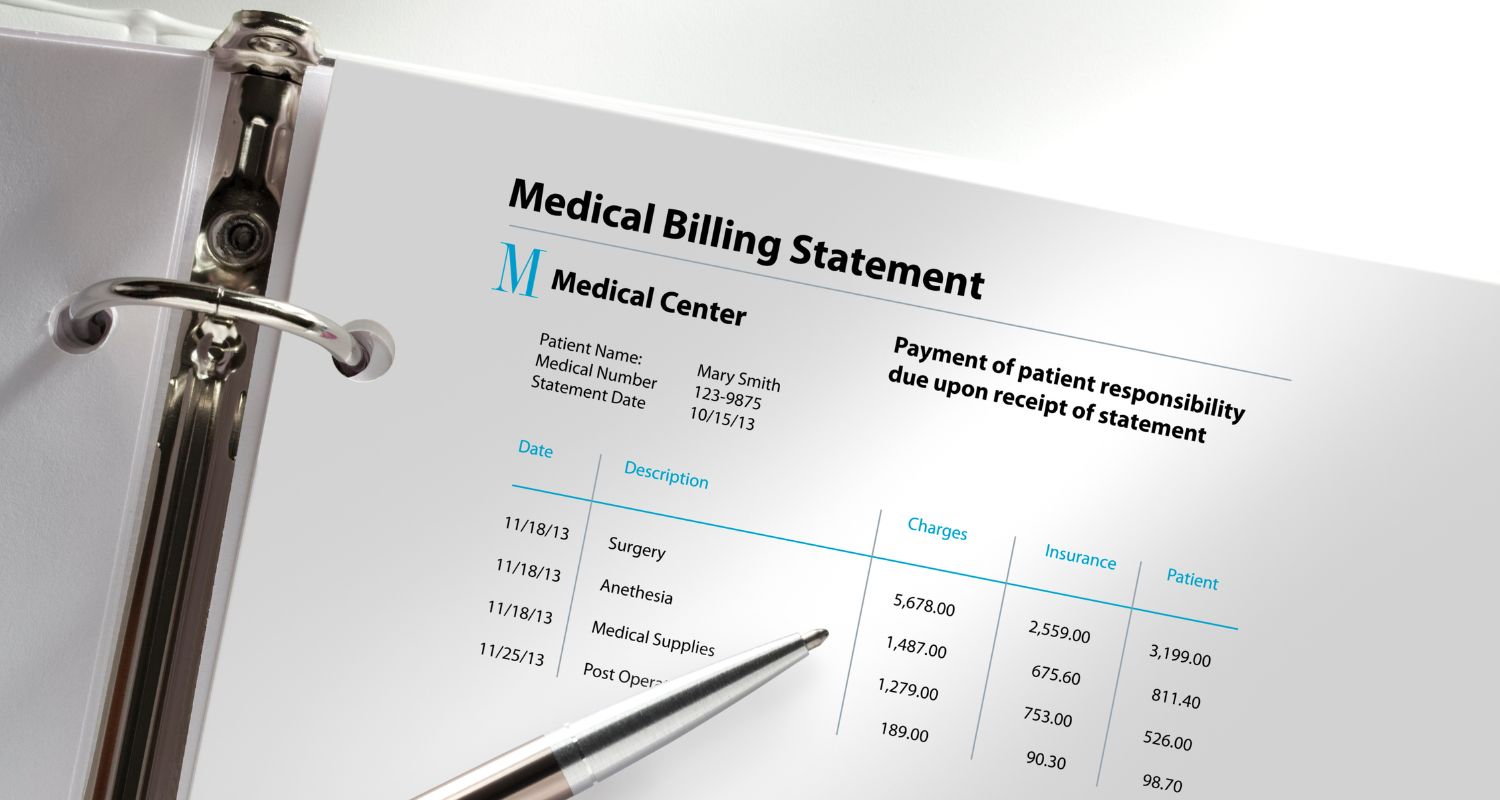
The medical bill consists of the following parts:
- Statement Date: The date on which the bill was created.
- Account number: A unique number assigned to a patient, which they must verify when contacting the billing office or when paying online.
- Service date: A column containing the date on which each medical service was provided.
- Description: A short explanation of each itemized service or supply on the bill.
- Charges: The full price of services, prior to insurance billing.
- Billed charges: The total amount ultimately charged, either to the patient or the insurance provider.
- Adjustment: The amount the healthcare provider has waived.
- Insurance payments: The amount already paid by the insurance provider.
- Patient payments: The amount for which the patient is responsible.
- Balance / Amount due: The outstanding balance owed to the healthcare provider.
- Payable to: The entity to which payment should be submitted—either the provider’s office, or their billing company.
An additional and significant part of the bill is the Explanation of Benefits, or EOB. This document is sent by the insurance provider to the patient after any claim is submitted by a healthcare provider. It explains which treatments were covered by the insurance company and which others are left for the patient to pay directly. The receipt of these documents has caused much dissatisfaction among patients over the years, as they are often full of surprises about just what services or supplies are not covered under the patient’s insurance plan. They may also reflect coding errors on the part of the provider, leading to miscommunication and confusion.
Solving the Problems With Medical Billing
Given the current complexity of our private insurance system, the billing process is not likely to become less complicated in the near term. Still, there are some steps that healthcare providers can take to improve communication with patients regarding billing. With patients more engaged throughout the process, we can ensure that they are not blindsided by charges they were not expecting.
- Frontline Staff Must Be Familiar With Billing and Insurance Protocols: Patients are unlikely to interact directly with billing staff at a hospital. This may even be unlikely in smaller practices. However, if the front desk personnel with whom patients do interact have some basic knowledge about the billing process, they can help answer patients’ questions. The more people patients encounter who don’t know how to answer their questions about billing, the more frustrating the experience is for them.
- Always Verify Eligibility in Advance: Check in advance whether a patient’s insurance company will cover a specific treatment or supply. When a patient expects to be covered for an expensive treatment, and is then denied, ending up responsible for thousands or tens of thousands of dollars they were not expecting, they are not likely to be satisfied.
- Discuss Eligibility With Patients: Print the eligibility document from the patient’s insurance provider so you can go over it together. If a service is not covered, it is a good idea to tell them that before providing it.
- Create a Sample Bill: Have an example of what a bill will look like, so patients can get familiar with the layout and terms before they receive it in the mail.
- Provide a Glossary: Whether on your website or in physical form, explain the terms your patients will encounter on their medical bill. This will help inspire trust that you understand the billing process and can account for all charges on their bill.
The best solution for your medical billing woes is to find a good third party to help. At Healthcare Revenue Group, we don’t just mail bills. We optimize your EMR system (such as eClinicalWorks, NextGen and ModMed) to streamline and maximize your revenue opportunities. We recommend growing your practice, removing the pain points in your billing cycle, and reducing denied claims to as little as 2%. Contact Healthcare Revenue Group today to talk about how we can save you time and money at your audiology practice, podiatry clinic, or other medical facility.
